What is Crohn’s Disease?
Crohn’s disease is a chronic inflammatory bowel disease that affects the digestive tract. It is characterized by inflammation of the lining of the digestive tract, which can lead to a wide range of symptoms. The disease can occur anywhere in the digestive tract, from the mouth to the anus, but most commonly affects the small intestine and colon.
Definition of Crohn’s Disease
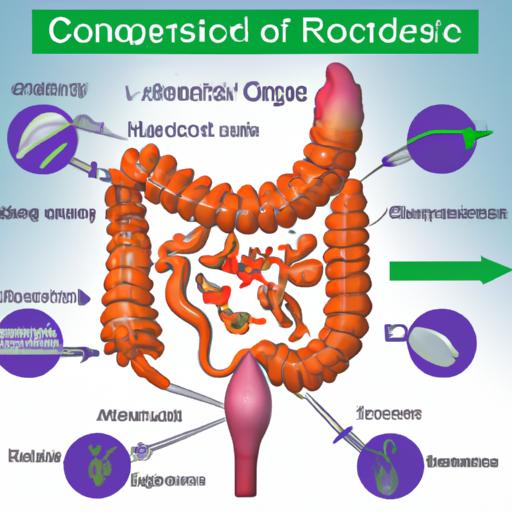
Crohn’s disease is part of a group of conditions known as inflammatory bowel disease (IBD). The disease is often confused with another IBD, ulcerative colitis, but the two conditions are distinct. While ulcerative colitis only affects the colon, Crohn’s disease can affect any part of the digestive tract.
Crohn’s disease causes inflammation that can penetrate the entire thickness of the bowel wall. This inflammation can result in a range of symptoms, including abdominal pain, diarrhea, fever, and weight loss. The severity of the symptoms varies from person to person, and some people with Crohn’s disease may experience long periods of remission.
Causes of Crohn’s Disease
The exact cause of Crohn’s disease is unknown, but researchers believe that a combination of genetic, environmental, and immune system factors may play a role in its development.
Genetic factors are thought to be an important component in the development of Crohn’s disease. Studies have shown that people with a family history of the disease are more likely to develop it themselves.
Environmental factors, such as diet and stress, may also contribute to the development of Crohn’s disease. Certain foods, such as dairy products, high-fat foods, and spicy foods, may trigger symptoms in some people. Stress can also exacerbate symptoms.
The immune system also appears to play a role in the development of Crohn’s disease. In people with the disease, the immune system mistakenly attacks the lining of the digestive tract, leading to inflammation.
Causes of Crohn’s Disease
In addition to genetic and environmental factors, the immune system also plays a role in the development of Crohn’s disease. In people with the disease, the immune system mistakenly attacks the lining of the digestive tract, leading to inflammation.
One theory suggests that the immune system may be responding to a viral or bacterial infection in the digestive tract, triggering an autoimmune response. However, no specific pathogen has been identified as the cause of Crohn’s disease.
Other factors that may contribute to the development of Crohn’s disease include smoking, nonsteroidal anti-inflammatory drugs (NSAIDs), and oral contraceptives. Smoking appears to increase the risk of developing the disease and can also worsen symptoms. NSAIDs and oral contraceptives have been linked to an increased risk of developing Crohn’s disease, but the evidence is not conclusive.
Symptoms of Crohn’s Disease
The symptoms of Crohn’s disease can vary widely from person to person and depend on the location of the inflammation in the digestive tract. Common symptoms of the disease include:
- Abdominal pain and cramping
- Diarrhea
- Rectal bleeding
- Fatigue
- Weight loss
- Loss of appetite
In some cases, complications may arise as a result of the disease, such as intestinal strictures (narrowing of the intestine), fistulas (abnormal connections between organs), and abscesses (pockets of pus). These complications can cause additional symptoms, such as nausea, vomiting, and fever.
Symptoms of Crohn’s disease can also differ between adults and children. In children, the disease may cause delayed growth and sexual development, as well as pain and tenderness in the abdomen. In adults, the disease may cause joint pain, skin problems, and inflammation in other parts of the body.
Diagnosis and Treatment of Crohn’s Disease
Early diagnosis and treatment of Crohn’s disease can help manage symptoms and prevent complications. The diagnosis of Crohn’s disease typically involves a combination of medical history, physical examination, and diagnostic tests.
Medical history and physical examination: The doctor will ask about the patient’s symptoms and perform a physical examination to check for signs of inflammation and other abnormalities.
Diagnostic tests: A variety of tests may be used to diagnose Crohn’s disease, including blood tests, stool tests, imaging tests (such as X-rays, CT scans, and MRI), and endoscopic procedures (such as colonoscopy and upper endoscopy).
Medications are the primary treatment for Crohn’s disease. The choice of medication depends on the severity and location of the disease. Medications used to treat Crohn’s disease include anti-inflammatory drugs, immunosuppressants, and biologics. Anti-inflammatory drugs, such as corticosteroids and aminosalicylates, can reduce inflammation and relieve symptoms. Immunosuppressants, such as azathioprine and methotrexate, can suppress the immune system and reduce inflammation. Biologics, such as infliximab and adalimumab, can target specific proteins in the immune system to reduce inflammation.
In severe cases, surgery may be necessary. Surgery may involve removing a diseased portion of the digestive tract or creating an ostomy, a surgical opening in the abdomen that allows waste to pass out of the body.
Living with Crohn’s Disease
Crohn’s disease is a chronic condition that requires ongoing management. While there is no cure for the disease, there are many strategies that can help manage symptoms and improve quality of life.
Coping strategies for managing symptoms include stress management techniques, such as deep breathing and meditation, and avoiding trigger foods that can exacerbate symptoms. It is also important to get enough rest and exercise regularly.
Lifestyle changes can also help manage Crohn’s disease. A healthy diet that is low in fat and high in fiber can help reduce inflammation and improve digestive function. Staying hydrated and getting enough sleep are also important.
Support resources are available for patients and their families. These resources may include support groups, counseling services, and educational materials. It is important to talk to a healthcare provider about available resources and to seek out support from family and friends.